
Knee Replacement Surgery
Types of Knee Replacements

Total knee arthroplasty, is a surgical procedure in which a damaged or worn-out knee joint is replaced with an artificial implant. It is commonly performed for severe arthritis (such as osteoarthritis, Rheumatoid arthritis or post traumatic arthritis) or knee injuries that cause chronic pain and mobility issues.
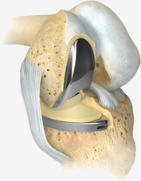
Uni-compartmental knee replacement or Partial Knee Replacement is a surgical procedure where only the damaged part of the knee joint is replaced with an artificial implant, rather than replacing the entire knee. It is typically an option for patients with osteoarthritis that is limited to one compartment of the knee.
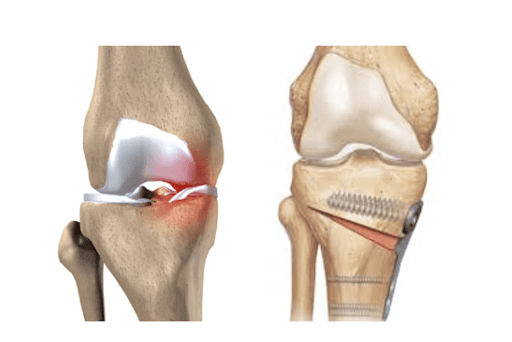
A High Tibial Osteotomy (HTO) is a surgical procedure used to treat knee osteoarthritis, particularly in younger, active patients with misalignment of the knee joint. It is commonly performed for medial compartment osteoarthritis, where the inner part of the knee wears down due to excessive weight-bearing stress.