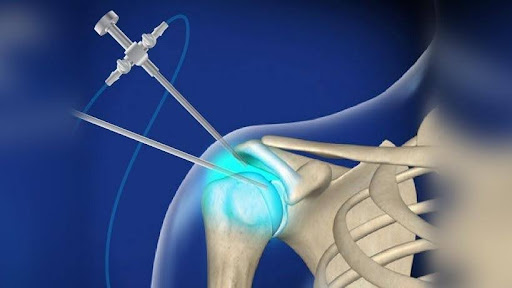
Shoulder Arthroscopy
Types of Shoulder Arthroscopies

A rotator cuff tear is a common shoulder injury that affects the group of four muscles and tendons responsible for stabilizing and moving the shoulder joint. It can result from acute injury (such as a fall or heavy lifting) or degenerative wear and tear over time, especially in older adults or athletes who perform repetitive overhead movements. Types of Rotator Cuff Tears –
– Partial Tear – The tendon is damaged but not completely severed.
– Complete Tear – The tear in the tendon is completely.
Shoulder Impingement Syndrome is a condition where the tendons or bursa in the shoulder become compressed or irritated, leading to pain and reduced mobility. It often occurs due to repetitive overhead movements, poor posture or muscle imbalances.


Also called as adhesive capsulitis, is a condition that causes pain, stiffness and reduced range of motion in the shoulder joint. It usually develops gradually and can take months or even years to fully resolve.
Also called as Bankart lesion is an injury to the anterior-inferior labrum of the shoulder joint, usually caused by an anterior shoulder dislocation. It occurs when the ball of shoulder joint forcefully pushes against the labrum, tearing it from the socket rim of the shoulder blade.
